Peer Reviewed Scholarly Articles on Femoral Artery Use for Cvp Monitoring
- Research
- Open Access
- Published:
Measuring the ratio of femoral vein diameter to femoral artery diameter past ultrasound to estimate volume condition
BMC Cardiovascular Disorders book 21, Article number:506 (2021) Cite this article
Abstract
Groundwork
Currently, the accustomed effective method for assessing blood volume status, such as measuring fundamental venous pressure level (CVP) and mean pulmonary artery pressure (mPAP), is invasive. The purpose of this report was to explore the feasibility and validity of the ratio of the femoral vein diameter (FVD) to the femoral avenue bore (FAD) for predicting CVP and mPAP and to summate the cut-off value for the FVD/FAD ratio to help judge a patient'southward fluid book status.
Methods
In this study, 130 patients were divided into 2 groups: in grouping A, the FVD, FAD, and CVP were measured, and in group B, the FVD, FAD, and mPAP were measured. Nosotros measured the FVD and FAD by ultrasound. We monitored CVP by a central venous catheter and mPAP by a Swan-Ganz floating catheter. Pearson correlation coefficients were calculated. The best cut-off value for the FVD/FAD ratio for predicting CVP and mPAP was obtained according to the receiver operating feature (ROC) curve.
Results
The FVD/FAD ratio was strongly correlated with CVP (R = 0.87, P < 0.0000) and mPAP (R = 0.73, P < 0.0000). Co-ordinate to the ROC curve, an FVD/FAD ratio ≥ 1.495 had the best test characteristics to predict a CVP ≥ 12 cmHtwoO, and an FVD/FAD ratio ≤ one.467 had the best test characteristics to predict a CVP ≤ x cmHtwoO. An FVD/FAD ratio ≥ 2.03 had the best test characteristics to predict an mPAP ≥ 25 mmHg. Co-ordinate to the simple linear regression bend of the FVD/FAD ratio and CVP, when the predicted CVP ≤ 5 cmH2O, the FVD/FAD ratio was ≤ 0.854.
Conclusion
In this study, the measurement of the FVD/FAD ratio obtained via ultrasound was strongly correlated with CVP and mPAP, providing a not-invasive method for quickly and reliably assessing blood volume status and providing expert clinical support.
Groundwork
In humans, blood volume is an of import cistron affecting the stability of haemodynamics, and an imbalance in blood volume can atomic number 82 to a variety of critical clinical weather. On the one mitt, excess volume tin lead to oedema, ascites, and an increase in extracellular volume. On the other hand, insufficient volume tin can cause multiple organ dysfunction syndrome (MODS). Therefore, assessing volume condition is disquisitional for treating disease. Blood volume status can exist assessed invasively or not-invasively. There are many invasive assessment methods, such as the measurement of central venous pressure (CVP) and mean pulmonary avenue force per unit area (mPAP). CVP is influenced by a number of factors (including thoracic, pericardial, and abdominal pressures and the specification of operational measurements) [1]. Every bit an indicator of fluid management, CVP sometimes cannot directly reflect blood book and sometimes may mislead handling decisions [i, two]. mPAP is an important alphabetize for evaluating pulmonary circulation volume status [3]. It is invasively measured with a pulmonary artery catheter (PAC), which needs to be monitored in an intensive care unit (ICU) and cannot provide fast and effective back up for clinical work [four]. Moreover, there are certain risks associated with these invasive methods. Complications related to the utilize of a PAC include those associated with venipuncture, such as arteriovenous fistula, pneumothorax, and thrombosis; those associated with catheterization, such equally arrhythmia; time-related complications of the PAC in the cardiovascular system, such as infection; and incorrect interpretation or utilize of exported information [4]. Given the above shortcomings of invasive assessment methods, a non-invasive, rapid, and effective method for assessing blood volume status is urgently needed.
Amidst the non-invasive evaluation methods that have been explored, measuring the junior vena cava (IVC) diameter with ultrasound is considered a reliable evaluation method with a good correlation with book status [5,6,7,viii]. The IVC diameter and its collapsibility index (IVC-CI) can be measured past ultrasound to evaluate CVP [9, ten]. However, the accuracy of measuring the IVC diameter via ultrasound is sometimes afflicted by certain factors, such as abdominal trauma, increased intra-intestinal force per unit area, ventricular wrinkle, obesity, and the patient'due south trunk position during measurement [five, 11]. Furthermore, measuring the IVC diameter by ultrasound is not every bit like shooting fish in a barrel to obtain every bit that for the superficial vein, and the requirements for surveyors and ultrasonic instruments are higher [six]. mPAP is an important indicator of haemodynamic monitoring and is of great significance for the diagnosis and treatment of some pulmonary diseases. Currently, well-nigh non-invasive assessments are performed by echocardiography, but most of them are based on the peak velocity of tricuspid regurgitation; for patients without tricuspid regurgitation, mPAP cannot be measured past this method [12, 13].
In recent years, scholars have explored some other non-invasive method for evaluating CVP: measurement of the femoral vein diameter (FVD) by ultrasound [fourteen, 15]. Although experiments take suggested that the FVD has a good correlation with CVP, private FVDs vary greatly and are affected by age, sex activity, height, body mass index, and other factors [16]. Therefore, to avert the influence of these factors, nosotros adopted the FVD/femoral artery bore (FAD) ratio in this study and explored its correlation with CVP and mPAP.
Materials and methods
Written report design
This prospective report was conducted in the intensive care unit of the Fourth Affiliated Hospital of Harbin Medical University in China. The report was approved by a hospital committee (ethical approval number: 2021-SCILLSC-x), and informed consent was obtained from the patient or authorized person. The inclusion criteria were as follows: patients over xviii years of age who required haemodynamic monitoring, for example, multiple organ failure, shock, heart failure, myocardial infarction, acute pulmonary oedema, acute pulmonary embolism, etc. The exclusion criteria were as follows: (a) patients with a correct atrium or right ventricle tumour; (b) patients with severe stenosis of the pulmonary valve or tricuspid valve; (c) patients with serious malformation of the pulmonary artery; (d) patients with thrombocytopenia or other serious clotting disorders; (due east) patients with a peel infection at the puncture site; (f) patients receiving mechanical ventilation; and (g) patients with lower extremity artery/vein thrombosis, significant lower extremity avenue plaque, lower extremity artery occlusion, inferior vena cava filter implantation, lower extremity varicose veins, or aortic stenosis.
Two highly trained doctors separately performed puncture and ultrasound examinations to minimize operational errors. The doctors performing the ultrasound test were unaware of the values of CVP and mPAP. The patient was in the supine position throughout the ultrasound test and haemodynamic monitoring. Nosotros used an EPIQ7 ultrasound machine (Phillips, United states of america) to measure the FVD and FAD.
First of all, twenty normal subjects were randomly selected, and their FVD and FAD were measured to determine the baseline FVD/FAD ratio. Then, the 130 patients were divided into two groups: Grouping A included patients requiring primal venous catheter placement in ICU, such equally shock, right heart failure, long-term infusion or intravenous hypertrophic therapy, etc. Group B included patients requiring Swan-Ganz floating catheter implantation in ICU, such as pulmonary oedema, pulmonary hypertension, and left heart failure, etc. In group A, the FVD, FAD, and CVP were measured. In grouping B, the FVD, FAD, and mPAP were measured.
Ultrasound measurement method
An ultrasound probe was used to first detect the bifurcation position of the femoral artery, and then the probe was retracted proximally. The visual field of the bifurcation disappeared until the probe entered the master branch of the femoral avenue, and the femoral artery and vein could exist observed simultaneously. Nether normal conditions, pulsation is an indication of the femoral artery, and its companion is the femoral vein (Fig. one). The mean FVD and FAD (3–5 diametral lines in different directions) were measured, so the patient was asked to coughing or perform Valsalva manoeuvres. Changes in the femoral vein were observed within one-half a minute, and the FVD was measured again (mainly used for FVD less than FAD). The FVD/FAD ratio and the FVD/FAD ratio after coughing (exFVD/FAD) were obtained.
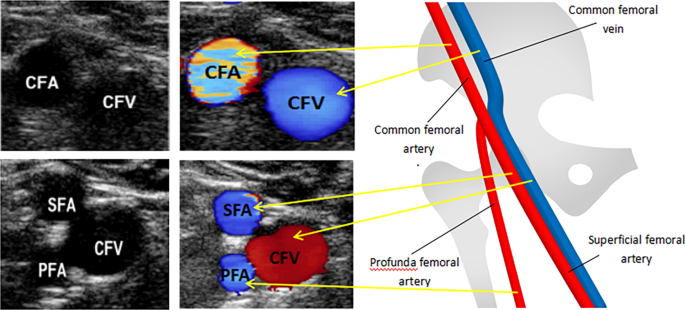
The images of femoral avenue and vein were measured by ultrasound
Haemodynamic monitoring
Afterward placing the central venous catheter/Swan-Ganz floating catheter through the correct internal jugular vein, the pressure sensor was connected at the opening of the central venous catheter/Swan-Ganz floating catheter and was linked to the monitor. The pressure sensor was placed on the level of the patient'south axillary midline. Subsequently the sensor was zeroed successfully, the values of CVP and mPAP were recorded.
Statistical assay
All the data were input and analysed with R 4.0.2 software. The results are expressed as the hateful ± standard deviation (SD). P < 0.05 was considered statistically significant. Multiple linear regression was used to analyse the human relationship between multiple independent variables and dependent variables. The Pearson correlation coefficient was used to analyse the relationship between the FVD/FAD ratio and CVP/mPAP. Simple linear regression was used to analyse the variable dependence. The receiver operating feature (ROC) curve was used to find the cut-off value.
Results
The study included 130 patients. At that place were 32 males and 33 females in group A and 28 males and 37 females in group B. In group A, the mean age was 65.5 ± 10.2 years, the hateful FVD/FAD ratio was ane.54 ± 0.thirty, and the mean CVP was 13.22 ± four.11 cmH2O, the hateful exFVD/FAD ratio for patients with the FVD/FAD ratio ≤ ane is i.23 ± 0.10. In grouping B, the mean age was 67.3 ± 10.3 years, the mean FVD/FAD ratio was ii.00 ± 0.32, and the mean mPAP was 25.63 ± 4.96 mmHg. The mean FVD/FAD ratio of twenty normal subjects was one.18 ± 0.04. The mean exFVD/FAD ratio of twenty normal subjects was ane.52 ± 0.09.
The FVD/FAD ratio, historic period and sex were independent variables, CVP and mPAP were taken every bit dependent variables, and multiple linear regression analysis was performed (Table 1). Assay of variance (ANOVA) was conducted, and the results are shown in Table 2. Age and sex had no pregnant effect on CVP and mPAP (P > 0.05). The FVD/FAD ratio was an influential gene for CVP and mPAP (P < 0.05). Therefore, simple linear regression was carried out with the FVD/FAD ratio as the only independent variable and CVP and mPAP as the dependent variables.
Figure 2 shows the simple linear regression bend of the FVD/FAD ratio and CVP. Linear regression showed that the FVD/FAD ratio was correlated with CVP (R = 0.87, P < 0.0000). The following regression equation was obtained: CVP = 11.9665 × (FVD/FAD) − 5.2147 (F: 197.4, P < 0.0000). The adjusted R-square was 0.7542.
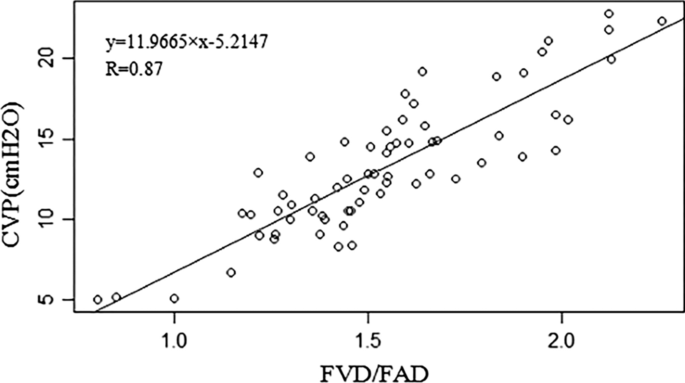
Correlation between the FVD/FAD ratio and CVP. FVD femoral vein diameter, FAD femoral avenue diameter, CVP central venous pressure level
Figure 3 shows the uncomplicated linear regression curve of the FVD/FAD ratio and mPAP. Linear regression showed that the FVD/FAD ratio was correlated with mPAP (R = 0.73, P < 0.0000). The following regression equation was obtained: mPAP = eleven.479 × (FVD/FAD) + 2.643(F: 75.93, P < 0.0000). The adjusted R-foursquare was 0.5393. However, when the FVD/FAD ratio was greater than 2.0, the adjusted R-square reached 0.6068.
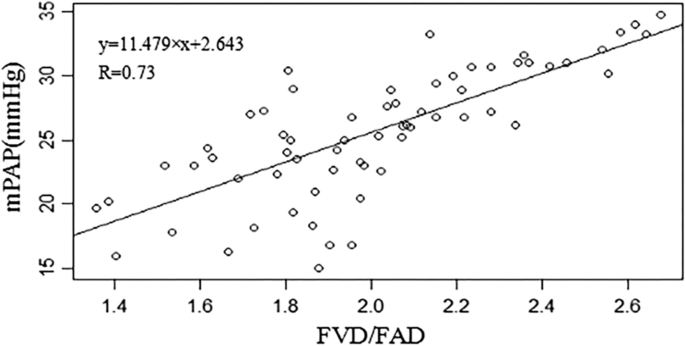
Correlation betwixt the FVD/FAD ratio and mPAP. FVD femoral vein diameter, FAD femoral artery diameter, mPAP mean pulmonary artery pressure
Figure 4 shows the area under the curve (AUC) of diverse CVP values predicted by the FVD/FAD ratio. For prediction of CVP ≥ 12 cmHtwoO past the FVD/FAD ratio, the AUC was 0.945 (95% CI, 0.891–0.998). The all-time FVD/FAD ratio cut-off values were obtained co-ordinate to the generated ROC bend. An FVD/FAD ratio ≥ one.495 had the best test characteristics to predict a CVP ≥ 12 cmHtwoO (sensitivity 87%; specificity 96%; positive predictive value 97%; negative predictive value 83%). For prediction of CVP ≤ x cmH2O past the FVD/FAD ratio, the AUC was 0.896 (95% CI, 0.819–0.974). An FVD/FAD ratio ≤ 1.467 had the best exam characteristics to predict a CVP ≤ 10 cmH2O (sensitivity 100%; specificity 71%; positive predictive value 46%; negative predictive value 100%). Co-ordinate to the simple linear regression curve of the FVD/FAD ratio and CVP, when the predicted CVP ≤ 5 cmH2O, the FVD/FAD ratio was ≤ 0.854.
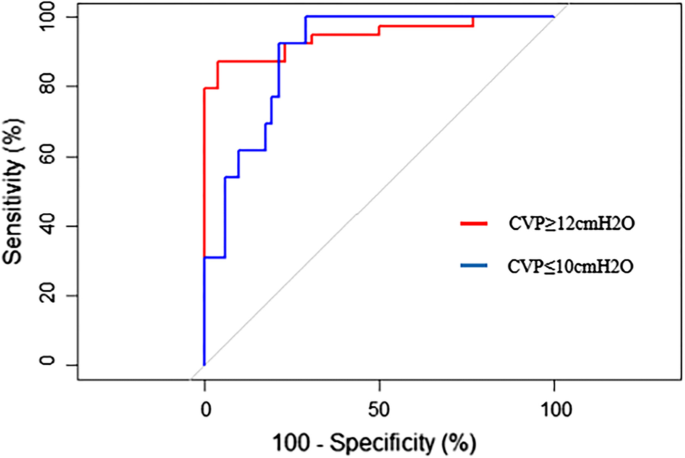
Receiver operating feature curve for prediction of diverse CVP values past the FVD/FAD ratio
Effigy v shows the AUC of the mPAP value predicted by the FVD/FAD ratio. For prediction of mPAP ≥ 25 mmHg by the FVD/FAD ratio, the AUC was 0.889 (95% CI, 0.811–0.967). An FVD/FAD ratio ≥ ii.03 had the best exam characteristics to predict an mPAP ≥ 25 mmHg (sensitivity 74%; specificity 100%; positive predictive value 100%; negative predictive value 87%).
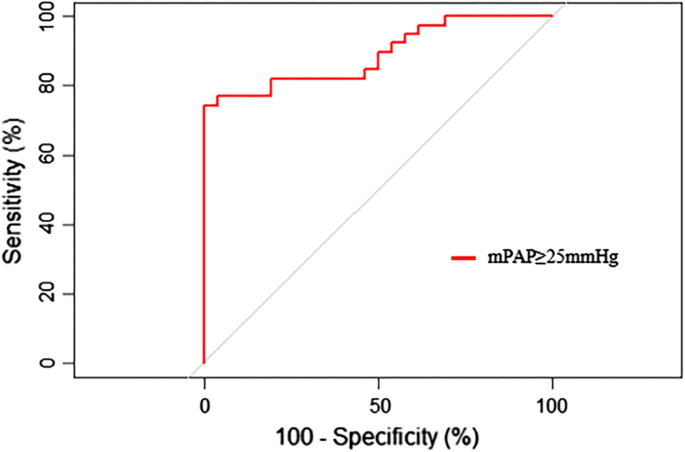
Receiver operating characteristic curve for prediction of mPAP value by the FVD/FAD ratio
Discussion
Several studies have reported the evaluation of CVP past ultrasound measurement of the IVC or internal jugular vein (IJV) [17,18,19,20]. In a written report by Nik Muhamad NA et al., the IVC bore at end expiration was better at predicting CVP than the IJV height [21]. In a study by Prekker ME et al., the maximal IVC diameter was better at predicting CVP than the IJV aspect ratio [6]. However, information technology is a challenge to perform loftier-quality IVC measurements via ultrasound due to factors such as abdominal gas, abdominal dressings, or poor audio-visual windows [22, 23]. Other studies have estimated mPAP by measuring the velocity of pulmonary regurgitation at the start of diastole, just this is difficult to mensurate, and changes in the structure of the right ventricle make it more difficult to mensurate [24, 25].
Nosotros performed baseline measurements in the normal population. Most of the claret in the normal human being vascular system (approximately 65%) is in the veins, and most of the blood that flows to the lower extremities via the femoral artery returns nearly equally to the femoral vein. This was also confirmed by the close equivalence of FVD and FAD under ultrasound observation in normal subjects. Therefore, it tin be inferred that if the FVD is significantly greater than the FAD, information technology can prove venous system volume overload; if the baseline FVD is slightly smaller than the FAD and FV fails to expand effectively afterwards cough, information technology tin can prove that the patient's blood volume is low. Therefore, book condition can be easily, quickly and accurately judged by authentic measurement of the FVD and FAD. Femoral artery and vein are mayor vessels, running close to the skin fifty-fifty in overweight personssuperficial vessels, easy to measure out under ultrasound. Notwithstanding, in patients with venous insufficiency, the book of the femoral vein increased significantly [26], so we excluded the patients with venous insufficiency in this study.
In this study, nosotros studied some other not-invasive method for volume status assessment: the FVD/FAD ratio. CVP and mPAP were predicted by the FVD/FAD ratio. According to the R values obtained from this experiment, the FVD/FAD ratio was strongly correlated with CVP (R = 0.87) and mPAP (R = 0.73). In the written report by Ciozda W et al., the authors summarized the correlation between the IVC diameter and the IVC-CI measured by ultrasound and CVP or right atrial pressure (RAP) that had been published in recent years [5]. The correlation coefficient R values between the ultrasound measurements of the maximum IVC diameter and CVP or RAP ranged from 0.35 to 0.86, with 57% having an R value between 0.5 and 0.78. The correlation coefficient R values between ultrasound measurements of IVC-CI and CVP or RAP ranged from − 0.27 to − 0.76, among which 62% were betwixt − 0.5 and − 0.76. The correlation coefficient R between the FVD/FAD ratio measured past ultrasound and CVP in this experiment was 0.87. The FVD/FAD ratio was slightly amend than the IVC in the correlation with CVP. The FVD/FAD ratio in this study was used to evaluate non only venous indicators simply also arterial indicators.
In the unproblematic linear equation established between the FVD/FAD ratio and CVP, the adjusted R-foursquare was 0.7542, which means that 75.42% of the CVP variance was affected past the FVD/FAD ratio. In the uncomplicated linear equation of the FVD/FAD ratio and mPAP, the adjusted R-square was 0.5393, which means that 53.93% of the variance in mPAP was due to the FVD/FAD ratio. When the FVD/FAD ratio was greater than 2.0, the adjusted R-foursquare was 0.6068, which means that 60.68% of the mPAP variance was due to the FVD/FAD ratio. In this study, we performed two sets of ROC analyses: (a) In this report, the all-time cut-off value of the FVD/FAD ratio for predicting a CVP ≥ 12 cmH2O was 1.495. The best cut-off value of the FVD/FAD ratio for predicting a CVP ≤ 10 cmH2O was 1.467. In previous studies, CVP ≤ 10 cmHiiO was selected equally the node for ROC bend analysis [half dozen, 14]. Although there was a small number of CVP ≤ 5 cmH2O measurements, we adamant that an FVD/FAD ratio ≤ 0.854 predicted a CVP ≤ 5 cmH2O through the simple linear regression curve of the FVD/FAD ratio and CVP. When FVD/FAD ratio ≤ 1, the mean exFVD/FAD ratio was 1.23 ± 0.10, which was far lower than the exFVD/FAD ratio of normal subjects. This suggests that the exFVD/FAD ratio is helpful for the diagnosis of hypovolemia. (b) In this report, the all-time cut-off value of the FVD/FAD ratio for predicting an mPAP ≥ 25 mmHg was 2.03. The specificity and positive predictive value reached 100%, indicating that when the FVD/FAD ratio was ≥ 2.03, all mPAP measurements according to the PAC were ≥ 25 mmHg. Although the FVD/FAD ratio in this written report could not wholly and accurately predict mPAP, the FVD/FAD ratio could be a skillful screen for pulmonary hypertension.
There are some limitations in this study. First, we preferred high CVP groups in this study because some patients with hypovolemia were already receiving fluid therapy at the time of measurement. Therefore, there may be some deviations in the estimation and prediction of low CVP groups. Second, the sample size of our study was small, and the selected population was relatively homogeneous, so the results may not be representative of all populations. Therefore, we volition increase the written report of hypovolemic patients in the follow-up written report to further verify the effectiveness of this method.
In conclusion, this study showed that the FVD/FAD ratio could accurately assess blood volume status and had sure clinical awarding value for diagnosing center failure, assessing astute internal blood loss, diagnosing pulmonary hypertension, and so on.
Conclusions
In this study, the measurement of the FVD/FAD ratio obtained via ultrasound was strongly correlated with CVP and mPAP. There was a linear relationship betwixt the FVD/FAD ratio and CVP or mPAP. The exFVD/FAD ratio is helpful for the diagnosis of hypovolemia. Moreover, the FVD/FAD has a screening effect on patients with loftier mPAP.
Availability of data and materials
The datasets used and analysed during the current study are bachelor from the corresponding author on reasonable asking.
Abbreviations
- CVP:
-
Fundamental venous force per unit area
- mPAP:
-
Mean pulmonary artery pressure
- FVD:
-
Femoral vein diameter
- FAD:
-
Femoral artery diameter
- MODS:
-
Multiple organ dysfunction syndrome
- PAC:
-
Pulmonary artery catheter
- ICU:
-
Intensive care unit
- IVC:
-
Inferior vena cava
- IVC-CI:
-
Junior vena cava collapsibility index
- ROC:
-
Receiver operating feature
- AUC:
-
Expanse under the curve
- IJV:
-
Internal jugular vein
- RAP:
-
Correct atrial pressure level
References
-
De Backer D, Vincent JL. Should nosotros measure the central venous pressure to guide fluid management? Ten answers to 10 questions. Crit Care. 2018;22(one):43. https://doi.org/10.1186/s13054-018-1959-three.
-
Marik PE, Baram M, Vahid B. Does cardinal venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of vii mares. Chest. 2008;134(1):172–8. https://doi.org/ten.1378/chest.07-2331.
-
Job Force for Diagnosis and Treatment of Pulmonary Hypertension of European Social club of Cardiology (ESC); European Respiratory Guild (ERS); International Society of Heart and Lung Transplantation (ISHLT), Galiè N, Hoeper MM, Humbert 1000, Torbicki A, Vachiery JL, Barbera JA, Beghetti M, Corris P, Gaine Southward, Gibbs JS, Gomez-Sanchez MA, Jondeau G, Klepetko W, Opitz C, Peacock A, Rubin L, Zellweger K, Simonneau One thousand. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2009;34(6):1219–63. https://doi.org/10.1183/09031936.00139009
-
Evans DC, Doraiswamy VA, Prosciak MP, Silviera M, Seamon MJ, Rodriguez Funes V, Cipolla J, Wang CF, Kavuturu Due south, Torigian DA, Cook CH, Lindsey DE, Steinberg SM, Stawicki SP. Complications associated with pulmonary artery catheters: a comprehensive clinical review. Scand J Surg. 2009;98(four):199–208. https://doi.org/10.1177/145749690909800402.
-
Ciozda Due west, Kedan I, Kehl DW, Zimmer R, Khandwalla R, Kimchi A. The efficacy of sonographic measurement of inferior vena cava diameter equally an approximate of central venous force per unit area. Cardiovasc Ultrasound. 2016;14(1):33. https://doi.org/10.1186/s12947-016-0076-ane.
-
Prekker ME, Scott NL, Hart D, Sprenkle Dr., Leatherman JW. Point-of-care ultrasound to estimate central venous pressure: a comparing of three techniques. Crit Care Med. 2013;41(3):833–41. https://doi.org/10.1097/CCM.0b013e31827466b7.
-
Sekiguchi H, Seaburg LA, Suzuki J, Astorne WJ, Patel As, Keller AS, Gajic O, Kashani KB. Fundamental venous force per unit area and ultrasonographic measurement correlation and their associations with intradialytic agin events in hospitalized patients: a prospective observational written report. J Crit Intendance. 2018;44:168–74. https://doi.org/x.1016/j.jcrc.2017.x.039.
-
Zengin S, Al B, Genc S, Yildirim C, Ercan S, Dogan M, Altunbas G. Function of inferior vena cava and correct ventricular diameter in assessment of volume status: a comparative written report: ultrasound and hypovolemia. Am J Emerg Med. 2013;31(5):763–7. https://doi.org/10.1016/j.ajem.2012.10.013.
-
Stawicki SP, Braslow BM, Panebianco NL, Kirkpatrick JN, Gracias VH, Hayden GE, Dean AJ. Intensivist utilise of manus-carried ultrasonography to measure out IVC collapsibility in estimating intravascular book status: correlations with CVP. J Am Coll Surg. 2009;209(1):55–61. https://doi.org/ten.1016/j.jamcollsurg.2009.02.062.
-
Zanobetti M, Prota A, Coppa A, Giordano L, Bigiarini S, Nazerian P, Innocenti F, Conti A, Trausi F, Vanni Due south, Pepe G, Pini R. Can not-invasive ventilation modify cardinal venous pressure? Comparison between invasive measurement and ultrasonographic evaluation. Intern Emerg Med. 2017;12(8):1279–85. https://doi.org/10.1007/s11739-016-1574-8.
-
Bano South, Qadeer A, Akhtar A, Ata Ur-Rehman HM, Munawar K, Hussain SW, Khan MT, Zafar R. Measurement of internal jugular vein and mutual carotid avenue bore ratio past ultrasound to guess central venous force per unit area. Cureus. 2018;x(3):e2277. https://doi.org/10.7759/cureus.2277.
-
Kasai H, Matsumura A, Sugiura T, Shigeta A, Tanabe N, Yamamoto M, Miwa H, Ema R, Sakao S, Tatsumi K. Hateful pulmonary artery pressure level using echocardiography in chronic thromboembolic pulmonary hypertension. Circ J. 2016;80(5):1259–64. https://doi.org/10.1253/circj.CJ-xv-1080.
-
Berger M, Haimowitz A, Van Tosh A, Berdoff RL, Goldberg E. Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol. 1985;half dozen(2):359–65. https://doi.org/10.1016/s0735-1097(85)80172-8.
-
Cho RJ, Williams DR, Leatherman JW. Measurement of femoral vein bore by ultrasound to guess central venous force per unit area. Ann Am Thorac Soc. 2016;13(1):81–5. https://doi.org/10.1513/AnnalsATS.201506-337BC.
-
Malik A, Akhtar A, Saadat Southward, Mansoor Southward. Predicting central venous force per unit area by measuring femoral venous bore using ultrasonography. Cureus. 2016;8(11):e893. https://doi.org/10.7759/cureus.893.
-
Fronek A, Criqui MH, Denenberg J, Langer RD. Common femoral vein dimensions and hemodynamics including Valsalva response as a function of sex, age, and ethnicity in a population report. J Vasc Surg. 2001;33(5):1050–six. https://doi.org/10.1067/mva.2001.113496.
-
Ilyas A, Ishtiaq W, Assad S, Ghazanfar H, Mansoor S, Haris M, Qadeer A, Akhtar A. Correlation of IVC diameter and collapsibility index with key venous pressure in the cess of intravascular book in critically ill patients. Cureus. 2017;9(ii):e1025. https://doi.org/10.7759/cureus.1025.
-
Martin LD, Ziegelstein RC, Howell EE, Martire C, Hellmann DB, Hirsch GA. Hospitalists' ability to use hand-carried ultrasound for primal venous force per unit area estimation after a brief training intervention: a pilot report. J Hosp Med. 2013;eight(12):711–4. https://doi.org/10.1002/jhm.2103.
-
Huguet R, Fard D, d'Humieres T, Brault-Meslin O, Faivre 50, Nahory Fifty, Dubois-Randé JL, Ternacle J, Oliver L, Lim P. Iii-dimensional inferior vena cava for assessing central venous force per unit area in patients with cardiogenic stupor. J Am Soc Echocardiogr. 2018;31(nine):1034–43. https://doi.org/ten.1016/j.echo.2018.04.003.
-
Parenti N, Scalese Chiliad, Palazzi C, Agrusta F, Cahill J, Agnelli G. Part of internal jugular vein ultrasound measurements in the cess of cardinal venous force per unit area in spontaneously breathing patients: a systematic review. J Acute Med. 2019;9(2):39–48. https://doi.org/10.6705/j.jacme.201906_9(2).0001.
-
Nik Muhamad NA, Safferi RS, Robertson CE. Internal jugular vein height and inferior vena cava diameter measurement using ultrasound to determine cardinal venous force per unit area: a correlation study. Med J Malaysia. 2015;lxx(2):63–6.
-
Jassim HM, Naushad VA, Khatib MY, Chandra P, Abuhmaira MM, Koya SH, Ellitthy MSA. IJV collapsibility index vs IVC collapsibility index by betoken of care ultrasound for estimation of CVP: a comparative study with straight estimation of CVP. Open Admission Emerg Med. 2019;eleven:65–75. https://doi.org/ten.2147/OAEM.S176175.
-
Naghipour B, Faridaalaee G. Correlation betwixt cardinal venous pressure and inferior vena cava sonographic bore; Determining the all-time anatomic location. Emerg (Tehran). 2016;iv(2):83–7.
-
Kanda T, Fujita M, Iida O, Masuda One thousand, Okamoto Southward, Ishihara T, Nanto K, Shiraki T, Takahara Thou, Sakata Y, Uematsu G. Novel echocardiographic approach to the authentic measurement of pulmonary vascular resistance based on a theoretical formula in patients with left heart failure—pilot study. Circ J. 2015;79(xi):2408–13. https://doi.org/ten.1253/circj.CJ-fifteen-0575.
-
、Howard LS, Grapsa J, Dawson D, Bellamy K, Chambers JB, Masani ND, Nihoyannopoulos P, Simon R Gibbs J. Echocardiographic assessment of pulmonary hypertension: standard operating procedure. Eur Respir Rev. 2012;21(125):239–48. https://doi.org/10.1183/09059180.00003912. Erratum in: Eur Respir Rev. 2012 Dec 1;21(126):370. PMID: 22941889.
-
Kahle B, Hennies F, Hummel S, Petzoldt D. Quantitative venous severity scoring using the venous arterial flow alphabetize by duplex sonography. Dermatol Surg. 2002;28(10):937–41. https://doi.org/10.1046/j.1524-4725.2002.02073.10.
Acknowledgements
The authors thank the patients and their families for their participation and cooperation in this report.
Funding
This work was supported by a grant from the National Natural Science Foundation of China Project [Grant No. 81670381 awarded to Bingchen Liu]. The funders accept no role in study design, information collection and analysis, manuscript preparation or publication decisions.
Author information
Affiliations
Contributions
BC-Fifty was responsible for the conception and design of the research and for providing technical guidance. L-10 was responsible for ultrasonic guidance and ultrasonic image collection. Zh-M wrote the get-go draft and added important intellectual content. JX-Yard, YH-S, and JY-L contributed to information drove and analysis. YP-B, HY-C, and Fifty-Due west were responsible for literature retrieval. Threescore-S modified the chart. Last draft read and canonical by all authors.
Respective author
Ethics declarations
Ethics approving and consent to participate
Blessing was obtained from the ethics commission of Harbin Medical University. The procedures used in this written report attach to the tenets of the Declaration of Helsinki. The written informed consent was obtained from all patients or authorized persons.
Consent for publication
Not applicable.
Competing interests
The authors declare that at that place is no disharmonize of involvement in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open up Admission This article is licensed nether a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in whatsoever medium or format, as long as you requite advisable credit to the original author(southward) and the source, provide a link to the Creative Commons licence, and betoken if changes were made. The images or other third political party material in this article are included in the commodity'south Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is non included in the article's Creative Commons licence and your intended apply is not permitted past statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/past/4.0/. The Creative Eatables Public Domain Dedication waiver (http://creativecommons.org/publicdomain/cypher/one.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and Permissions
Almost this article
Cite this commodity
Ma, Z., Gai, J., Sun, Y. et al. Measuring the ratio of femoral vein bore to femoral avenue diameter past ultrasound to estimate book condition. BMC Cardiovasc Disord 21, 506 (2021). https://doi.org/x.1186/s12872-021-02309-7
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/ten.1186/s12872-021-02309-vii
Keywords
- Femoral vein diameter
- Femoral artery diameter
- CVP
- mPAP
- Volume status
- Pulmonary hypertension
Source: https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-021-02309-7
0 Response to "Peer Reviewed Scholarly Articles on Femoral Artery Use for Cvp Monitoring"
Post a Comment